
|
|
Font Size:
|
||||
|
|
|
|
||||
Recent Changes in Treatment Patterns for Diagnosed or Treated High Cholesterol, 2018-19 to 2021-22
Statistical Brief #566 | September 2025 | Steven C. Hill, PhD, and Zhengyi Fang, MS
Highlights
- The annual average number of adults diagnosed or treated for high cholesterol rose from 76.4 million in 2018-19 to 84.2 million in 2021-22.
- Among adults ever diagnosed with or currently treated for high cholesterol in 2021-22, 56.6 percent obtained antihyperlipidemic medications, including 44.3 percent who also had check-ups or ambulatory visits for high cholesterol, and 12.3 percent who obtained medications but did not have visits.
- Adults with diagnosed or treated high cholesterol were more likely to have obtained medications without visits in 2021-22 (12.3%) than in 2018-19 (10.7%).
- The percentage of adults with diagnosed or treated high cholesterol who had no medical treatment increased from 19.3 percent in 2018-19 to 21.6 percent in 2021-22.
- In 2021-22, lack of medical treatment was three times as prevalent among adults ages 18 to 64 (31.1%), relative to adults aged 65 or older (10.6%) and was especially high for adults ages 18 to 64 who lacked a usual source of care (57.1%) or who were uninsured (64.6%).
Introduction
One in ten adults (10.0%) have high total cholesterol, and one in four (24.7%) have borderline high cholesterol.1 Poor diet, physical inactivity, smoking, obesity, diabetes, and genetics are risk factors for high cholesterol.2 Preventing high cholesterol could reduce health care expenditures on visits and medications to treat high cholesterol. Treating high cholesterol with diet, exercise, and medications can reduce the risk of coronary heart disease, including heart attack and stroke, which are serious health problems and expensive to treat.1,3 Among adults with diagnosed high cholesterol and those unaware of their high cholesterol, only half take medications.4,5
In this Statistical Brief, data from the Household Component of the Medical Expenditure Panel Survey (MEPS-HC) are used to estimate changes in patterns of treatment for adults with diagnosed and/or treated high cholesterol. Other data suggest more than a third of adults with high cholesterol were not aware they had it,5 but that population could not be included in this Brief. The treatments we examine in this Brief are use of antihyperlipidemic medications and ambulatory visits for high cholesterol, including primary care and some additional check-ups. We estimate the percentages of adults with the following treatment patterns: visits and drugs; drugs, no visits; visits, no drugs; and no medical treatment. Visits are important for establishing an effective medication regimen to control high cholesterol. Patients and pharmacies can ask providers to renew prescriptions without a visit. Treatment guidelines recommend testing cholesterol levels at least annually for patients with high cholesterol,6 and tests or counseling may have occurred during check-ups with primary care providers, cardiologists, and, for adults with diabetes, endocrinologists.7 All these check-ups were included as visits.
This Brief covers 2018 to 2022, a period of time that spans changes in recommended treatment of high cholesterol and use of statins, the most common antihyperlipidemic medications. The American Heart Association and other organizations jointly released new guidelines in November 20186 that may affect treatment during the period of time covered by the Brief. These guidelines included newly recommended (1) antihyperlipidemic agents besides statins, and (2) considering medication for some adults ages 20 to 39 with elevated low-density lipoprotein cholesterol. In August 2022, the U.S. Preventive Services Task Force recommended the use of statins to prevent cardiovascular disease (CVD) among adults ages 40 to 75 with a high risk of a CVD event (such as heart attack or stroke) and at least one risk factor for CVD, such as high cholesterol.8 The Task Force recommendations, however, were released late in the period of time covered by this Brief.
Average annual estimates for the civilian, noninstitutionalized population are from pooled years (2018-2019 and 2021-2022) to increase precision. All differences discussed in the text are statistically significant at the 0.05 level.
Findings
Adult population diagnosed or treated for high cholesterol (Figure 1)
In 2021-22, on average, 84.2 million adults per year were diagnosed with or treated for high cholesterol, including 45.2 million ages 20 to 64 ("nonelderly") and 39.0 million ages 65 and older ("elderly"). This number increased from 76.4 in 2018-19, with the largest increase among elderly adults, where there was an increase of 5.3 million (from 33.7 million).
Treatment Patterns (Figure 2)
Ambulatory visits for high cholesterol are comprised of (1) office, outpatient department, and emergency department visits for which the household respondent reported high cholesterol as a reason for the visit, and (2) among adults with high cholesterol, check-ups with primary care providers, cardiologists, and, for those who also had diabetes, endocrinologists. Among adults ever diagnosed or currently treated for high cholesterol in 2021-22, 44.3 percent both had ambulatory visits for high cholesterol and obtained antihyperlipidemic medications, 12.3 percent obtained medications but did not have visits, 21.8 percent had visits but did not obtain medications, and 21.6 percent had no medical treatment. More than half (56.6%) of adults, therefore, with diagnosed or treated high cholesterol obtained antihyperlipidemic medications in 2021-22, which was not statistically significantly different from 2018-19 (56.7%). However, the percentage who had medications, but no visits increased from 10.7 percent in 2018-19 to 12.3 percent in 2021-22, the percentage who had visits, but no medications decreased from 24.0 percent in 2018-19 to 21.8 percent in 2021-22, and the percentage who had no medical treatment increased from 19.3 percent in 2018-19 to 21.6 percent in 2021-22. Not shown in the figure are the 0.1 percent of the adults who had hospital stays or home health visits for high cholesterol, but not ambulatory visits or medications.
Treatment Patterns by Age (Figure 3)
In 2021-22, among adults with diagnosed or treated high cholesterol, 31.1 percent of nonelderly adults (ages 20-64) did not receive medical treatment, which was almost three times the rate among elderly adults (ages 65 and older), 10.6 percent. Elderly adults were less likely to have visits but no medications (16.9% versus 26.0%) and more likely than nonelderly adults to both have visits and obtain medications (58.8% versus 31.7%) and obtain medications without visits (13.5% versus 11.2%).
Among elderly adults with diagnosed or treated high cholesterol, treatment patterns changed between 2018-19 and 2021-22 in the same manner as the adult population as a whole. Specifically, the percent using medications did not change significantly. However, the percent with medications but no visits increased, the percent with visits but no medications decreased, and the percent with no treatment increased. Among nonelderly adults with diagnosed or treated high cholesterol, 28.5 percent were not medically treated in 2018-19, rising to 31.1 percent in 2021-22.
Nonelderly Adults with Diagnosed but Not Medically Treated High Cholesterol (Figure 4)
Among nonelderly adults with diagnosed or treated high cholesterol, Figure 4 shows the percentage not medically treated by demographic and other subgroups. In 2021-22, more than half (57.1%) of nonelderly adults with diagnosed or treated high cholesterol who lacked a usual source of care had no medical treatment for their high cholesterol. Similarly, nearly two-thirds (64.6%) of nonelderly adults who were uninsured the entire calendar year had no medical treatment for their high cholesterol.
Among nonelderly adults with diagnosed or treated high cholesterol, lack of medical treatment increased from 2018-19 to 2021-22 for two groups. For those with family incomes at least 200 percent of the Federal Poverty Line, the share that lacked medical treatment rose from 27.8 percent in 2018-19 to 30.6 percent in 2021-22. For those who had public insurance coverage, the share that lacked medical treatment rose from 23.2 percent in 2018-19 to 28.6 percent in 2021-22. None of the differences between the two time periods were statistically significant for any of the other subgroups examined in Figure 4.
Elderly Adults with Diagnosed but Not Medically Treated High Cholesterol (Figure 5)
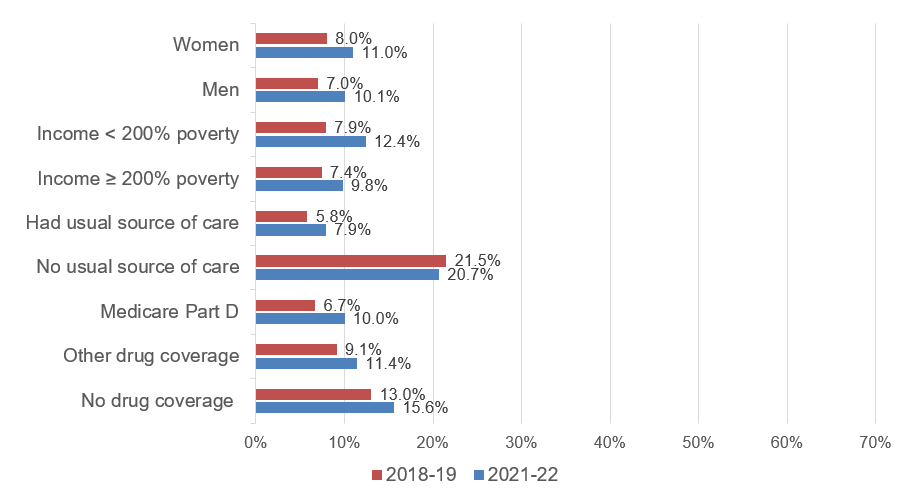
Among elderly adults with diagnosed or treated high cholesterol, Figure 5 shows the percentage not medically treated by demographic and other subgroups. Comparing Figures 4 and 5, elderly adults were less likely than non-elderly adults to lack medical treatment for their high cholesterol in both time periods for all categories for which a comparison can be made.
In 2021-22, one in five (20.7%) elderly adults with diagnosed or treated high cholesterol who lacked a usual source of care had no medical treatment for their high cholesterol, which is more than twice the rate for those who had a usual source of care (7.9%). In 2021-22, elderly adults without insurance coverage for prescription medicines were more likely to lack medical treatment for high cholesterol (15.6%) than those with Medicare Part D (10.0%) and those with private drug coverage or through the Veterans Administration (11.4%).
The increase from 2018-19 to 2021-22 in the share that lacked medical treatment was statistically significant for many elderly subgroups: women (8.0% to 11.0%), men (7.0% to 10.1%), with family incomes below 200 percent of the Federal Poverty Line (7.9% to 12.4%), with family incomes at or above 200 percent of the Federal Poverty Line (7.4% to 9.8%), had a usual source of care (5.8% to 7.9%), and had Medicare Part D drug coverage (6.7% to 10.0%).
Data Source
The estimates shown in this Statistical Brief are based on data from the MEPS for 2018, 2019, 2021, and 2022: (a) the Medical Conditions Files (H207, H214, H231, H241), (b) Condition-Event Link Files (H206IF1, H213IF1, H229IF1, H239IF1), (c) Office-Based Medical Provider Visits Files (H206G, H213G, H229G, H239G), (d) Outpatient Visits File (H206F, H213F, H229F, H239F), (e) Emergency Room Visits Files (H206E, H213E, H229E, H239E), (f) internal versions of the Prescribed Medicines Files (H206A, H213A, H229A, H239A), (g) Hospital Inpatient Stays Files (H206D, H213D, H229D, H239D), (h) Home Health Files (H206H, H213H, H229H, H239H), and (i) Full-Year Consolidated Data Files (H209, H216, H233, H243). These data files are publicly available from this site: https://meps.ahrq.gov/data_stats/download_data_files.jsp.
Definitions
Adults
Age 20 or older at the end of the calendar year (or on last date of MEPS eligibility if person was out of scope at the end of the year). This Brief starts with age 20 because the U.S. Preventive Services Task Force does not recommend screening asymptomatic children or adolescents for high cholesterol.8
Age groups
Elderly: Ages 65 or older at the end of the calendar year (or on last date of MEPS eligibility if person was out of scope at the end of the year).
Nonelderly: Ages 20 to 64 at the end of the calendar year (or on last date of MEPS eligibility if person was out of scope at the end of the year).
High cholesterol
This statistical brief combined two ways of identifying adults with high cholesterol.
Diagnosed high cholesterol. Assignment to this group was determined by an affirmative answer to "{Have/Has} {you/{PERSON} ever been told by a doctor or other health professional that {you/he/she} had high cholesterol?"
Treated high cholesterol. Adults were classified as treated for high cholesterol if they purchased any antihyperlipidemic agents during the calendar year or had one or more other healthcare events (office-based, hospital outpatient or emergency room visits, hospital inpatient stays, or home health care) where high cholesterol was reported as leading to or having been discovered during the event. Adults with diagnosed high cholesterol were also classified as treated if they had a check-up with a primary care physician (family practice, general practice, geriatrics, or internist medicine with no subspecialty specified), mid-level practitioner (nurse practitioner or physician assistant), cardiologist, or, if they had diabetes, endocrinologist.
Conditions reported by household respondents as leading to or having been discovered during events were not verified by medical professionals. MEPS-HC conditions reported by households were coded into International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes, which were then collapsed into Clinical Classifications Software Refined (CCSR) categories (see https://hcup-us.ahrq.gov/toolssoftware/ccsr/dxccsr.jsp for details). Conditions with CCSR code END010 (disorders of lipid metabolism) were used for this Brief.
Treated but not reported as ever diagnosed: This Brief included adults who reported treatment for high cholesterol but who did not report they had "ever been told by a doctor or other health professional that [they] had high cholesterol." Excluding them would not substantially increase the share of adults with high cholesterol who were not medically treated, as they comprised only 1 percent of the adult population ages 20 and over and 5 percent of the adults with diagnosed or treated high cholesterol.
Evidence suggests that adults who were treated but were not reported as ever diagnosed in fact had high cholesterol. For example, many adults in this group obtained drugs only indicated for high cholesterol.
Alternative definition of untreated high cholesterol: In this Brief, the definition of adults with untreated high cholesterol excludes adults who were unaware of their high cholesterol, who were not identified in the MEPS. Estimates from the National Health and Nutrition Examination Survey (NHANES) suggest the unaware comprise 38.5 percent of adults with high cholesterol,5 and including them would substantially increase the untreated population. The effects of including the unaware on trends and subgroups, however, are unknown.
The NHANES includes clinical measures of high cholesterol that are not available in the MEPS. Analyses of the NHANES define high cholesterol as measured low-density lipoprotein cholesterol 160mg/dL or higher5 or total cholesterol 200mg/dL or higher.1 These definitions cannot be replicated in the MEPS, which does not measure cholesterol levels.
Antihyperlipidemic agents
Each drug that was listed as purchased or otherwise obtained was assigned to one or more therapeutic classes in the Multum Lexicon therapeutic classification system from Cerner Multum, Inc. This system identifies the main therapeutic class of antihyperlipidemic agents considered in the report. Within this class, fibric acid derivatives, cholesterol absorption inhibitors, miscellaneous antihyperlipidemic agents, and antihyperlipidemic combinations were always included. However, bile sequestrants, PCSK9 inhibitors, and most statins were included only when the respondent reported either the sample member was ever diagnosed with high cholesterol or the drug was used to treat high cholesterol, because medications in these classes have multiple uses. For example, statins are also used for primary prevention of cardiovascular disease in adults with other risk factors for this condition.8
Treatment for high cholesterol
Adults with high cholesterol are classified into these mutually exclusive categories based on their reported events and antihyperlipidemic agents.
Visits and drugs: Obtained antihyperlipidemic medications and had either (1) ambulatory visits (office based, outpatient, and emergency room visits) for high cholesterol, or (2) primary care or cardiology check-ups, or, for adults with diabetes, endocrinology check-ups.
Visits, no drugs: Did not obtain antihyperlipidemic medications and had either (1) ambulatory visits (office based, outpatient, and emergency room visits) for high cholesterol, or (2) primary care or cardiology check-ups, or, for adults with diabetes, endocrinology check-ups.
Drugs, no visits: Obtained antihyperlipidemic agents and no visits for high cholesterol, no primary care or cardiology check-ups, and, for adults with diabetes, endocrinology check-ups.
No medical treatment: No events for high cholesterol, no primary care or cardiology check-ups, no endocrinology check-ups for adults with diabetes, and did not obtain antihyperlipidemic medications. These sample members may nonetheless have been treating their high cholesterol with diet, exercise, and other changes towards healthier lifestyles.
Among those who did not report visits, check-ups, or antihyperlipidemic agents, respondents rarely reported emergency room visits, hospital stays, or home health visits for high cholesterol, so this category is omitted from Figures 2 and 3.
Primary care, cardiology, and endocrinology check-ups contributed substantially to the share of adults with diagnosed high cholesterol with each type of treatment. Among those with visits and drugs, 70 percent had check-ups, but no visits linked to high cholesterol. Among those with visits and no drugs, 80 percent had check-ups but not visits linked to high cholesterol. When check-ups are excluded, 43.2 percent had medications and no visits, and 39.0 percent were medically untreated. When the medically untreated include those with check-ups but no visits reportedly for high cholesterol and no antihyperlipidemics, then the patterns of use by age and other characteristics are very similar to those in Figures 4 and 5, but the rates are higher.
Income
Each sample person was classified according to the total annual income of his or her family. Possible sources of income included annual earnings from wages, salaries, bonuses, tips, and commissions; business and farm gains and losses; unemployment and Worker's Compensation; interest and dividends; alimony, child support, and other private cash transfers; private pensions, individual retirement account (IRA) withdrawals, Social Security, and Department of Veterans Affairs payments; Supplemental Security Income and cash welfare payments from public assistance, Aid to Families with Dependent Children, and Aid to Dependent Children; gains or losses from estates, trusts, partnerships, S corporations, rent, and royalties; and a small amount of "other" income.
We report family income relative to the Federal Poverty Line (FPL), which varies with family size, age of the head of the family, and family composition. It is adjusted annually for inflation. For example, in 2022, the FPL for a family of 2 adults and 2 children was $29,678 annual income. Thus, twice the FPL was $59,356 in 2022.
Usual Source of Care
For each family member, MEPS ascertains whether there is a particular doctor's office, clinic, health center, or other place that the respondent usually visits if he/she is sick or needs advice about his/her health.
Insurance coverage for the nonelderly
Any private insurance: Individuals under age 65 were classified as having any private health insurance coverage if they had private insurance that provided coverage for hospital and physician care (including TRICARE, which is Armed Forces-related coverage) at some point during the year.
Public coverage only: Individuals under age 65 were considered to have public health insurance coverage if they were not covered by private insurance or TRICARE, and were covered by Medicare, Medicaid, the Veterans Administration, or other public hospital and physician coverage at some point during the year.
Uninsured all year: Individuals under age 65 who did not have health insurance coverage for the entire calendar year were classified as uninsured. The uninsured were defined as people not covered by Medicaid, Medicare, TRICARE, other public hospital/physician programs, private hospital/physician insurance, or insurance purchased through health insurance Marketplaces. People covered only by non-comprehensive state-specific programs (e.g., Maryland Kidney Disease Program) or private, single-service plans, such as coverage for dental or vision care only, or coverage for accidents or specific diseases, were considered uninsured.
Prescription drug coverage for the elderly
Medicare Part D: Individuals were classified as having Medicare Part D if they were covered by Medicare Part D or Medicaid at some point during the year.
Other drug coverage: Individuals were classified as having other drug coverage if they were not covered by Medicare Part D or Medicaid and were covered by private insurance that included drug coverage, TRICARE, or the Veterans Administration at some point during the year.
No drug coverage: Individuals who did not have drug coverage for the entire calendar year were classified as lacking drug coverage. This category includes people not covered by Medicare Part D, Medicaid, TRICARE, Veterans Administration, or private insurance with drug coverage at any time during the year.
About MEPS-HC
MEPS-HC is a nationally representative longitudinal survey that collects detailed information on health care utilization and expenditures, health insurance, and health status, as well as a wide variety of social, demographic, and economic characteristics for the U.S. civilian noninstitutionalized population. It is cosponsored by the Agency for Healthcare Research and Quality and the National Center for Health Statistics.
The following Methodology Reports contain information on the survey and sample designs for the MEPS Household and Medical Provider Components (HC and MPC, respectively). Data collected in these two components are jointly used to derive MEPS health care expenditure data.
Cohen, J. Design and Methods of the Medical Expenditure Panel Survey Household Component. MEPS Methodology Report No. 1. AHCPR Pub. No. 97-0026. Rockville, MD. Agency for Healthcare Policy and Research, 1997. http://meps.ahrq.gov/mepsweb/data_files/publications/mr1/mr1.pdf
Chowdhury, S.R., Machlin, S.R., Gwet, K.L. Sample Designs of the Medical Expenditure Panel Survey Household Component, 1996-2006 and 2007-2016. Methodology Report #33. January 2019. Agency for Healthcare Research and Quality, Rockville, MD. https://meps.ahrq.gov/data_files/publications/mr33/mr33.shtml
Machlin, S.R., Chowdhury, S.R., Ezzati-Rice, T., DiGaetano R., Goksel H., Wun L.M., Yu W., Kashihara D. Estimation Procedures for the Medical Expenditure Panel Survey Household Component. Methodology Report #24. September 2010. Agency for Healthcare Research and Quality, Rockville, MD. http://meps.ahrq.gov/mepsweb/data_files/publications/mr24/mr24.shtml
Mitchell, E., Ahrnsbrak, R., Soni, A., Machlin, S. Analyzing Medical Conditions in MEPS: User Guide (Part 1 of 2). Methodology Report #36. Rockville, MD: Agency for Healthcare Research and Quality; February 2023 https://meps.ahrq.gov/data_files/publications/mr36/mr36ug.shtml
Stagnitti, M.N., Machlin, S.R., Zodet, M.W., Saleska, E. Design, Methods, and Field Results of the Medical Expenditure Panel Survey Medical Provider Component (MEPS MPC) including the Medical Organizations Survey (MOS)-2016 Data Year. Methodology Report #32. October 2018. Agency for Healthcare Research and Quality, Rockville, MD. https://meps.ahrq.gov/data_files/publications/mr32/mr32.shtml
References
1 Martin, S.S., Aday, A.W., Allen, N.B., Almarzooq, Z.I., Anderson, C.A.M., Arora, P., Avery, C.L., Baker-Smith, C.M., Bansal, N., Beaton, A.Z., Commodore-Mensah, Y., Currie, M.E., Elkind, M.S.V., Fan, W., Generoso, G., Gibbs, B.B., Heard, D.G., Hiremath, S., Johansen, M.C., Kazi, D.S., Ko, D., Leppert, M.H., Magnani, J.W., Michos, E.D., Mussolino, M.E., Parikh, N.I., Perman, S.M., Rezk-Hanna, M., Roth, G.A., Shah, N.S., Springer, M.V., St-Onge, M.P., Thacker, E.L., Urbut, S.M., Van Spall, H.G.C., Voeks, J.H., Whelton, S.P., Wong, N.D., Wong, S.S., Yaffe, K., Palaniappan, L.P.; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Committee. 2025 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. 2025;151(8):e41-e660. doi: 10.1161/CIR.0000000000001303.
2 Centers for Disease Control and Prevention (CDC). Risk Factors for High Cholesterol. 2024 (Accessed April 28, 2025). https://www.cdc.gov/cholesterol/risk-factors/index.html
3 Centers for Disease Control and Prevention (CDC). Living with High Cholesterol. 2024 (Accessed May 2, 2025). https://www.cdc.gov/cholesterol/prevention/index.html
4 Wall, H.K, Ritchey, M.D., Gillespie, C., Omura, J.D., Jamal, A., George, M.G. Vital Signs: Prevalence of Key Cardiovascular Disease Risk Factors for Million Hearts 2022 — United States, 2011-2016. Morbidity and Mortality Weekly Report. 2018;67(35):983-991. https://www.cdc.gov/mmwr/volumes/67/wr/mm6735a4.htm
5 Sayed, A., Navar, A.M., Slipczuk, L., Ballantyne, C.M., Samad, Z., Lavie, C.J., Virani, S.S. Prevalence, Awareness, and Treatment of Elevated LDL Cholesterol in US Adults, 1999-2020. JAMA Cardiology. 2023 Dec 1;8(12):1185-1187. doi: 10.1001/jamacardio.2023.3931.
6 Grundy, S.M., Stone, N.J., Bailey, A.L., Beam, C., Birtcher, K.K., Blumenthal, R.S., Braun, L.T., de Ferranti, S., Faiella-Tommasino, J., Forman, D.E., Goldberg, R., Heidenreich, P.A., Hlatky, M.A., Jones, D.W., Lloyd-Jones, D., Lopez-Pajares, N., Ndumele, C.E., Orringer, C.E., Peralta, C.A., Saseen, J.J., Smith, S.C., Sperling, L., Virani, S.S., Yeboah, J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;139(25):e1082-e1143. doi: 10.1016/j.jacc.2018.11.002.
7 American Diabetes Association Professional Practice Committee. Cardiovascular Disease and Risk Management: Standards of Care in Diabetes, 2025. Diabetes Care. 2024;48(Supplement 1):S207-S238. doi: 10.2337/dc25-S010
8 US Preventive Services Task Force. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: Preventive Medication. 2022 (Accessed May 6, 2025). https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/statin-use-in-adults-preventive-medication
Suggested Citation
Hill, S.C., and Fang, Z. Recent Changes in Treatment Patterns for Diagnosed or Treated High Cholesterol, 2018-19 to 2021-22. Statistical Brief #566. AHRQ Publication No. 25-0087. September 2025. Agency for Healthcare Research and Quality, Rockville, MD. https://meps.ahrq.gov/data_files/publications/st566/stat566.shtml
AHRQ welcomes questions and comments from readers of this publication who are interested in obtaining more information about access, cost, use, financing, and quality of healthcare in the United States. We also invite you to tell us how you are using this Statistical Brief and other MEPS data and tools and to share suggestions on how MEPS products might be enhanced to further meet your needs. Please email us at MEPSProjectDirector@ahrq.hhs.govor send a letter to the address below:
Samuel H. Zuvekas, PhD, Acting Director
Center for Financing, Access and Cost Trends
Agency for Healthcare Research and Quality
5600 Fishers Lane, Mailstop 07W41A
Rockville, MD 20857
Figures
Figure 1. Average annual adult population diagnosed or treated for high cholesterol (millions), by age, 2018-19 and 2021-22
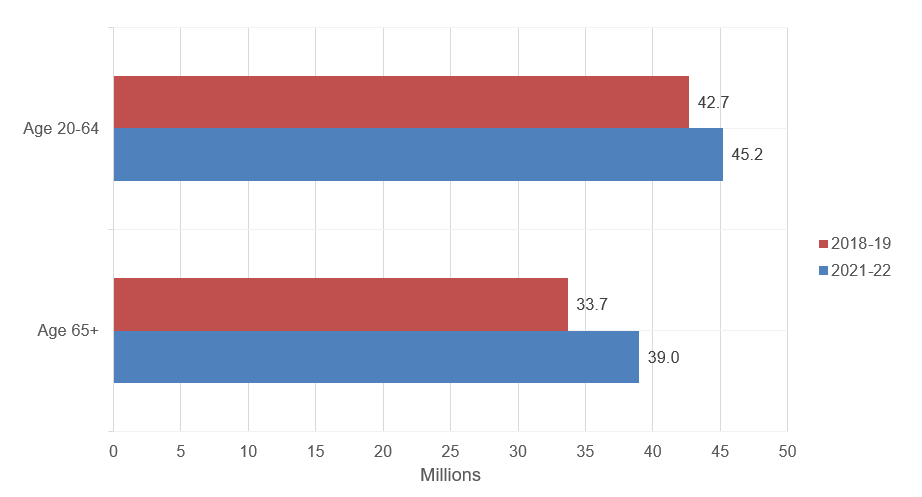
| 2018-19 (millions) | 2021-22 (millions) | |
|---|---|---|
| Age 20-64 | 42.7 | 45.2 |
| Age 65+ | 33.7 | 39.0 |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2018-19 and 2021-22.
Figure 2. Distribution of treatment patterns for adults with diagnosed or treated high cholesterol, 2018-19 and 2021-22
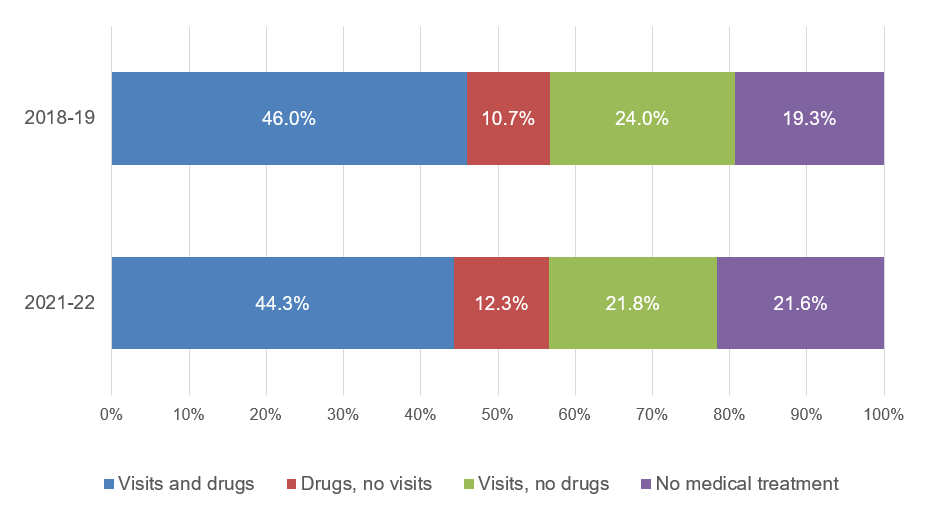
| 2018-19 | 2021-22 | |
|---|---|---|
| Visits and drugs | 46.0% | 44.3% |
| Drugs, no visits | 10.7% | 12.3% |
| Visits, no drugs | 24.0% | 21.8% |
| No medical treatment | 19.3% | 21.6% |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2018-19 and 2021-22.
Figure 3. Distribution of treatment patterns for adults with diagnosed or treated high cholesterol, by age, 2018-19 and 2021-22
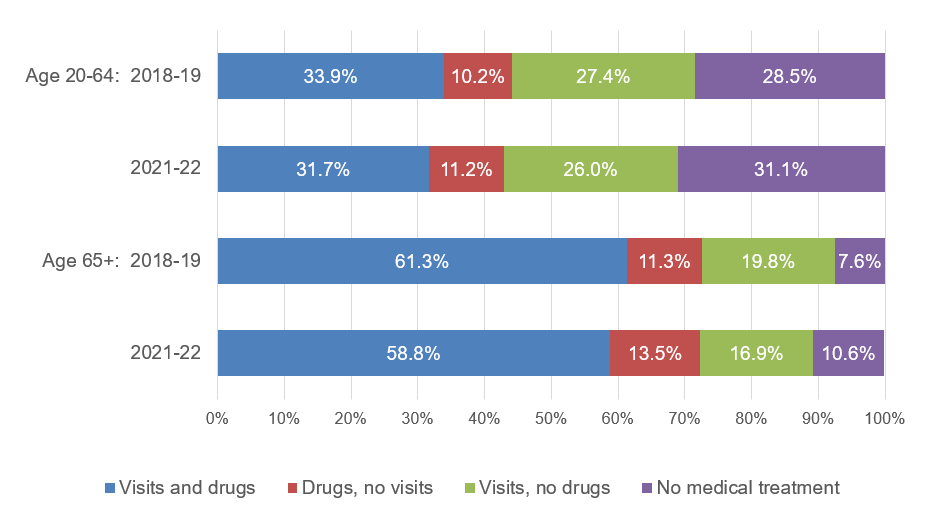
| Age 20-64 | Age 65+ | |||
|---|---|---|---|---|
| 2018-19 | 2021-22 | 2018-19 | 2021-22 | |
| Visits and drugs | 33.9% | 31.7% | 61.3% | 58.8% |
| Drugs, no visits | 10.2% | 11.2% | 11.3% | 13.5% |
| Visits, no drugs | 27.4% | 26.0% | 19.8% | 16.9% |
| No medical treatment | 28.5% | 31.1% | 7.6% | 10.6% |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2018-19 and 2021-22.
Figure 4. Among nonelderly adults with diagnosed or treated high cholesterol, percent whose high cholesterol was not medically treated, by subgroup, 2018-19 and 2021-22
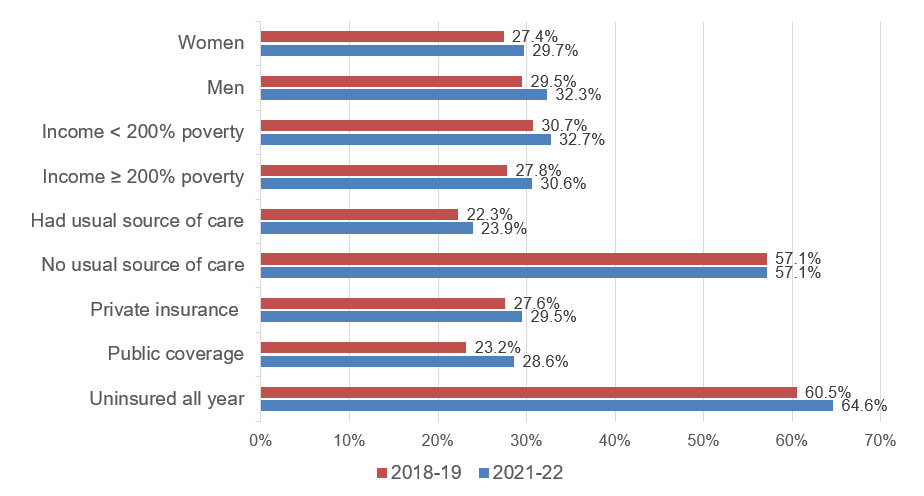
| 2018-19 | 2021-22 | |
|---|---|---|
| Women | 27.4% | 29.7% |
| Men | 29.5% | 32.3% |
| Income < 200% poverty | 30.7% | 32.7% |
| Income ≥ 200% poverty | 27.8% | 30.6% |
| Had usual source of care | 22.3% | 23.9% |
| No usual source of care | 57.1% | 57.1% |
| Private insurance | 27.6% | 29.5% |
| Public coverage | 23.2% | 28.6% |
| Uninsured all year | 60.5% | 64.6% |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2018-19 and 2021-22.
Figure 5. Among elderly adults with diagnosed or treated high cholesterol, percent whose high cholesterol was not medically treated, by subgroup, 2018-19 and 2021-22
| 2018-19 | 2021-22 | |
|---|---|---|
| Women | 8.0% | 11.0% |
| Men | 7.0% | 10.1% |
| Income < 200% poverty | 7.9% | 12.4% |
| Income ≥ 200% poverty | 7.4% | 9.8% |
| Had usual source of care | 5.8% | 7.9% |
| No usual source of care | 21.5% | 20.7% |
| Medicare Part D | 6.7% | 10.0% |
| Other drug coverage | 9.1% | 11.4% |
| No drug coverage | 13.0% | 15.6% |
Source: Agency for Healthcare Research and Quality, Medical Expenditure Panel Survey, Household Component, 2018-19 and 2021-22.
AHRQ Pub. No. 25-0087
September 2025


